How exactly do you know your blood type? How were people able to figure this information out? And why does knowing your blood type have so much importance within medicine? What’s the point of it? And why do we have different blood types anyway?
What is Blood Typing?
Blood typing is a test that is taken that identifies specific proteins (antigens) on your red blood cells, like A, B, Rh D, K, k, Kpa, Kpb, Fya, Fyb, Jka, Jkb, M, N, S, s, and U. This also is used to determine your ABO group, which is whether your blood type is A, B, AB, or O, and your Rh group, which is either positive or negative.
Your blood type is also inherited from your parents, just like your eye color, skin color, hair color, and so on. Having 2 parents with type O will result in their child having O as well. One parent with AB blood and the other with O will result in a child with either type A or type B blood. O + B = O or B and A + B = O, A, B, or AB. There’s many possibilities for a combination of blood types and their results.
How Does it Work?
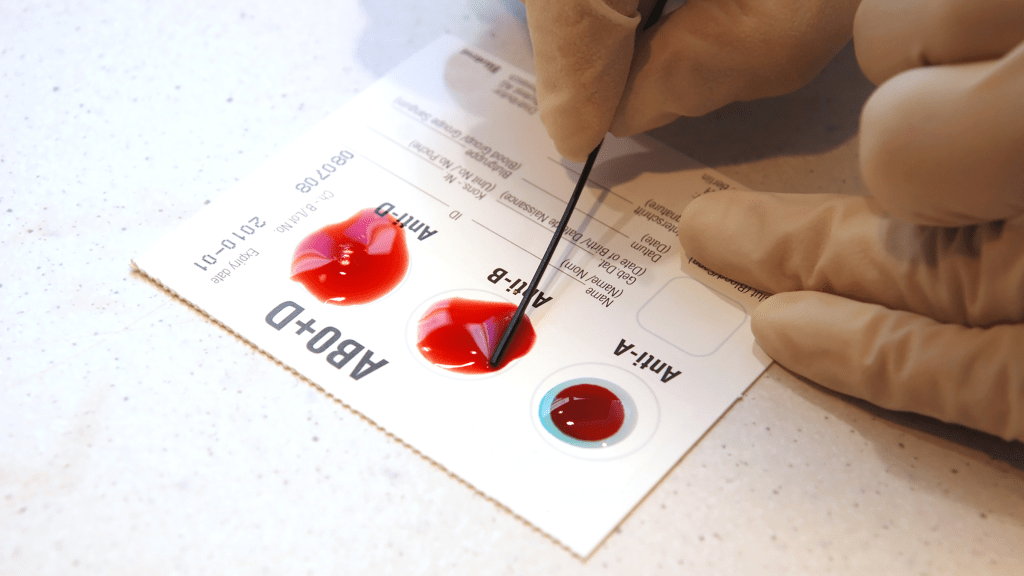
Of course, there’s a procedure involved within blood typing and the science behind how your blood type and Rh factor is determined. When given a blood sample, the blood is mixed with antibodies that are against both type A and type B, type A blood having anti-B antibodies, type B blood having anti-A antibodies, and type O having both of those antibodies. Based on which antibodies agglutinate, this determines what your blood type is. If only the anti-A antibodies clump together, you have type A blood, and the same way for B with anti-B antibodies agglutinating. If both anti-A and anti-B antibodies agglutinate, you have type AB blood. If neither of the antibodies agglutinate, that means you have type O blood.
Agglutinate?
The reason these antibodies agglutinate, aka “clump,” is because these antibodies are like keys that have a fitting lock, which is the matching antigen (specific sugar markers). When the anti-A antibodies come in contact with their matching antigen, the A antigens, they lock onto them, which crosslinks them into very visible clumps (hemagglutination). This is why receiving a blood transfusion with the wrong blood type is extremely dangerous and fatal
Blood Transfusion from the Wrong Blood Type
If someone with Type A blood receives a transfusion with Type B blood, acute hemolysis is very soon to follow in around an hour to receiving the wrong blood type. The recipient’s antibodies will begin to destroy the donor’s RBCs within the blood vessel due to the fact that Type A blood has Anti-B antibodies, which see these Type B antigens as foreign. These Anti-B antibodies will then agglutinate with these antigens. This becomes a signal to immune cells, like macrophages (a phagocytic cell), to phagocytize these clumped cells. It’s also a signal to the complement system to “punch holes” within them. When the Membrane Attack Complex (MAC) Formation inserts itself into the lipid bilayer of the RBC membrane, it develops a large, destructive pore or channel within said RBC, which then begins to cause the cell contents to leak out and water to rush into it. This leads to the swelling and eventual lysis (bursting) of the RBC.


Leave a comment